Marvin Webster iHuman Case Study
I. Introduction
- Marvin Webster iHuman Context
- The Marvin Webster iHuman case study is one of the most popular virtual simulations used by nursing and healthcare students in 2025.
- It focuses on realistic patient interactions, allowing learners to practice essential health assessment skills in a safe, guided environment.
- Marvin Webster iHuman is a standardized virtual patient within the iHuman platform designed to enhance critical thinking in clinical application.
- The case presents complex symptoms, requiring students to apply diagnostic reasoning, review study guides, and use structured approaches for patient care.
Overview of Marvin Webster iHuman
- Case Study Purpose
- The Marvin Webster iHuman case study challenges students to combine theoretical knowledge with clinical application.
- It ensures learners understand not just symptoms, but also underlying conditions, encouraging holistic health assessment.
- Key iHuman Learning Outcomes
- Mastery of patient interviewing and examination techniques.
- Improved documentation through interactive study guides.
- Application of evidence-based practice in analyzing Marvin Webster iHuman scenario.
- Why Does Marvin Webster iHuman Case Matter in 2025
- Among the various iHuman cases, Marvin Webster’s stands out for its balance of difficulty and relevance.
- It prepares nursing students for real-world challenges by simulating authentic patient encounters.
The Marvin Webster iHuman case study has become a cornerstone for nursing education in 2025, bridging classroom theory with practical clinical reasoning while leveraging study guides for structured learning.
Marvin Webster iHuman Simulation Case Overview
Problem Statement on Marvin Webster iHuman
- The patient is an 18-year-old presenting for evaluation of a dry cough and associated sore throat, myalgias, fatigue, and headache for the past several days.
- PMH is significant for a history of childhood asthma, a sick contact with similar symptoms (roommate), missed annual flu vaccine, and COVID booster.
- Physical exam shows a fever (38.3), tachycardia (108bpm), anterior cervical lymphadenopathy, and an erythematous pharynx.
Electronic Health Record on Marvin Webster iHuman-Week 2 ihuman.
Key Findings on case Marvin Webster iHuman (OLDCARTS)
- O – Onset
- Symptoms began 4 days ago after hanging out with friends.
- L – Location
- Sore throat (pharynx).
- Associated symptoms: cough, headache, and generalized fatigue.
- D – Duration
- Sore throat and other symptoms have been constant since the onset (4 days).
- Fatigue is also constant, not relieved by rest.
- C – Character
- Sore throat: painful, worsens with swallowing, better with steam/warm drinks.
- Cough: dry.
- Fatigue: described as severe, “feels like got run over by Shaquille O’Neal.”
- A – Aggravating Factors
- Sore throat aggravated by swallowing.
- No aggravating factors identified for fatigue or cough.
- R – Relieving Factors
- Sore throat relieved with steam and warm fluids.
- No relieving factors for fatigue or cough.
- T – Timing
- Continuous since onset (4 days).
- No specific diurnal variation reported.
- S – Severity
- Sore throat rated 8/10 in intensity.
- Fatigue severe, persistent.
- Headache and cough are not rated but implied as bothersome.
History of Present Illness
- Reason for Encounter: Dry cough, sore throat & fatigue.
- History of Present Illness: Marvin Webster, an 18-year-old male university student, presents with complaints of a sore throat, cough, headache, and fatigue. Symptoms began like a flu-like bug after a hangout with friends. The sore throat began 4 days ago at the same time as other symptoms, is constant, and feels better with steam and drinking something warm. It has a severity of 8 out of 10. He
describes the cough as dry and the fatigue as constant.
Past Medical History
- Past Medical History: Resolved childhood asthma.
- Hospitalizations / Surgeries: Denies hospitalization, minor or major surgeries.
Medications
- Denies herbal/OTC or prescription drug use.
Allergies
- Denies allergies to drugs, food, or environment.
Preventive Health
- Missed this year’s flu vaccine and COVID booster.
Family History
- Father (57) alive & healthy, mother (58) with a PMH on hypertension.
Social History
- Takes wine or beer occasionally after studying or on the weekends, active college student, denies tobacco smoking, denies illicit/recreational drug use.
Review of Systems
General
- Reports fatigue, denies chills, fevers, intentional/unintentional weight gain/weight loss, night sweats, generalized weakness, malaise, or changes in
appetite.
Integumentary / Breast
- Non-contributory.
HEENT / Neck
- Reports a headache, denies head trauma, dizziness, loss of central or peripheral vision, denies abnormal discharge from ears, denies pain or ringing in ears, loss of hearing, sores or ulcerations on the cheeks, tongue or gums.
- Denies difficulty closing or opening the jaw, difficulty swallowing, hoarseness, or loss of taste.
- Reports sore throat, denies recurrent nosebleeds, nasal discharge or loss of smell.
- Neck: denies pain with neck movement, swelling, or lumps in the neck.
Cardiovascular
- Denies swelling in face, upper or lower extremities, palpitations, chest pain, and inability to participate in physical activity or sports, or history of murmurs.
Respiratory
- Reports a dry cough, denies shortness of breath (SOB), difficulty in breathing (DIB), wheezing, reports missed last annual flu vaccine, denies second-hand smoke exposure.
Gastrointestinal
- Denies vomiting, nausea, blood in stool, constipation, diarrhea, changes in appetite, abdominal pain, black/tarry stools, greasy/ foul smelling stools.
Genitourinary
- Non-contributory
Musculoskeletal
- Reports myalgia, denies pain or swelling in the neck, back, joints, or upper or lower extremities. Denies problems with reaching, bending or standing.
Allergic / Immunologic
- Denies allergies to drugs, food, or environment.
Endocrine
- Non-contributory
Hematologic / Lymphatic
- Non-contributory
Neurologic
- Acknowledges headaches, denies dizziness, fainting, numbness or tingling in the face, upper or lower extremities, denies lightheadedness, seizures, or loss of consciousness.
Psychiatric
- Non-contributory
Physical Examination on Marvin Webster iHuman
General Appearance
AOX4, in no pain or respiratory distress, well-groomed with a good nutritional status.
Skin
Deferred.
HEENT / Neck
- No bruising or lesions, normocephalic.
- Eyes: PERRLA, no enopthalmos or exophthalmos, no evidence of intraocular bleeding or periorbital edema, retina intact bilaterally.
- Ears: No pain with pushing the tragus or movement of the pinna, no discharge, swelling or redness on structures of the inner or outer ear, hearing intact bilaterally, shiny, gray, and intact tympanic membrane, dark brown cerumen, absence of inflammation, fluid, or exudates around the inner ear and tympanic membrane.
- Nose/Mouth/Throat: No swelling in turbinates, bruising or bleeding, mucous membranes are pink & intact with no bleeding, erythematous pharynx, no tonsillar exudates.
- Neck: bilateral anterior cervical lymphadenopathy, no goiter, masses, or lumps, thyroid is symmetrical.
Cardiovascular
- PMI 5th intercostal space mid-clavicular line (MCL), S1 & S2 normal heart sounds, no gallops, murmurs, or rubs.
- Tachycardia (108bpm), regular, no pedal or facial edema, no gallops, murmurs, or rubs.
Chest / Respiratory
- No clubbing of nails, scars, lesions, or masses, chest wall is symmetrical, no palpable masses or lumps, bilateral clear lung sounds in all lobes, RR 16 at rest.
Abdomen
- Non-distended, soft, non-tender, no protruding tumors, lumps, or masses with percussion or palpation, active and present bowel sounds in all four abdominal quadrants, no rebound tenderness, fluid thrill, or shifting dullness.
Genitourinary / Rectal
- Deferred
Musculoskeletal / Osteopathic Structural Examination
- Deferred
Neurologic
- Deferred
Psychiatric
- Deferred
Lymphatic
- No pathologically enlarged lymph nodes.
Management Plan on Marvin Webster iHuman Case
Diagnostic Tests
- No additional tests are needed in this visit.
Medications
- Medication name: Acetaminophen 325mg tablets (Taaffe et al., 2024).
- SIG: Take 1 to 2 tablets by mouth 6 hourly for fevers, headaches, or myalgia.
- Disp: 24 tablets
- Refills: 0
- Medication name – Dextromethorphan HBr 20mg + Guaifenesin 400mg 20mL (Taaffe et al., 2024).
- Disp: 600mL
- Refills: 0
Suggested Consults/Referrals
- No consults are needed in this visit.
- Client Education
- Teach about influenza: It is a viral illness affecting the respiratory system and caused by the influenza virus. Its classical symptoms include: headache, a low-grade fever, chills, sore throat, a persistent dry cough, muscle aches, and fatigue (Taaffe et al., 2024). It is managed with OTC drugs to relieve symptoms, rest, and adequate hydration.
- Teach about hygiene: stay isolated until symptoms wane, wash hands frequently with clean running water and soap or alcohol-based hand sanitizers, practice cough etiquette by covering the mouth and nose with a tissue or elbow when coughing or sneezing (Taaffe et al., 2024).
- Teach about prescribed medications: acetaminophen is an antipyretic & analgesic that relieves fevers and headaches and is associated with side effects such as vomiting, abdominal cramping, and nausea. Dextromethorphan/Guaifenesin combination is an expectorant used to relieve cough & sore throat, with side effects including nausea and drowsiness.
Follow-up
- Return to this clinic in 14 days.
- Return for flu vaccine when current symptoms wane.
- Call 911 or visit the ED for chest pain, shortness of breath (SOB), wheezing, or difficulty in breathing (DIB) (Taaffe et al., 2024).
Reference
Taaffe, J., Ostrowsky, J. T., Mott, J., Goldin, S., Friede, M., Gsell, P., & Chadwick, C. (2024). Advancing influenza vaccines: A review of next-generation candidates and their potential for global health impact. Vaccine, 42(26), 126408. https://doi.org/10.1016/j.vaccine.2024.126408
SOAP Note on Marvin Webster iHuman
S – Subjective
- CC (Chief Complaint): “I have a sore throat, dry cough, fatigue, and headache for 4 days.”
- HPI: Marvin Webster is an 18-year-old male university student who presents with a 4-day history of sore throat, dry cough, headache, fatigue, and myalgia. Symptoms began after hanging out with friends. The sore throat is constant, painful (8/10), worsens with swallowing, and relieved by warm fluids/steam. Fatigue is persistent, not relieved by rest, and described as severe (“feels like got run over by Shaquille O’Neal”). Associated symptoms: dry cough and headache. Reports sick contact (roommate with similar symptoms).
- PMH: Childhood asthma (resolved).
- Medications: Denies OTC, prescription, or herbal use.
- Allergies: Denies drug, food, or environmental allergies.
- Preventive Health: Missed influenza vaccine and COVID booster.
- FH: Father (57) healthy; Mother (58) has hypertension.
- SH: Occasional alcohol use (beer/wine), denies smoking or illicit drugs. Active college student.
- ROS: Positive for fatigue, sore throat, myalgias, headache, and dry cough. Denies SOB, chest pain, nasal congestion, N/V/D, abdominal pain, or neurologic deficits.
O – Objective
- General: AOX4, well-groomed, no acute distress.
- Vitals: Temp 38.3°C (febrile), HR 108 bpm (tachycardic), RR 16, SpO₂ not recorded.
- HEENT/Neck: Normocephalic. Erythematous pharynx, no tonsillar exudates. Anterior cervical lymphadenopathy bilaterally. Eyes normal (PERRLA). Ears WNL. Mucous membranes intact.
- CV: Tachycardia, regular rhythm, S1/S2 normal, no murmurs, rubs, or gallops.
- Respiratory: Clear lung fields bilaterally, symmetrical chest wall movement, no wheezing or rales.
- Abdomen: Soft, non-tender, non-distended, bowel sounds present.
- Skin/Neuro/Psych/Lymphatic: Deferred except noted anterior cervical lymphadenopathy.
A – Assessment
- Primary Diagnosis: Viral Pharyngitis with Influenza-like illness.
- Differential Diagnoses:
- Influenza infection (given fever, fatigue, cough, myalgias, unvaccinated status).
- Streptococcal pharyngitis (sore throat, pharyngeal erythema, lymphadenopathy, but no exudates noted).
- COVID-19 infection (respiratory symptoms, missed booster, sick contact).
- Viral URI (generalized viral syndrome presentation).
P – Plan
- Diagnostics: No additional tests required at this visit.
- Medications:
- Acetaminophen 325mg PO q6h PRN fever, headache, or myalgia (Disp: 24 tabs, 0 refills).
- Dextromethorphan HBr 20mg + Guaifenesin 400mg PO q6h PRN cough (Disp: 600mL, 0 refills).
- Education:
- Discuss influenza: viral illness affecting the respiratory system; managed with OTC symptom relief, rest, and hydration.
- Infection control: self-isolate until symptoms resolve, practice frequent handwashing, cover mouth/nose when coughing or sneezing.
- Medication teaching: acetaminophen for fever/headache (side effects: nausea, abdominal discomfort). Dextromethorphan/Guaifenesin for cough (side effects: drowsiness, nausea).
- Follow-up:
- RTC in 14 days for re-evaluation.
- Return for influenza vaccination once recovered.
- Seek urgent care/ED if chest pain, SOB, wheezing, or worsening symptoms occur.
Differential Diagnosis – Marvin Webster iHuman Case
| Differential Diagnosis | Supporting Findings | Findings Against / Less Likely | Diagnostic Rationale |
|---|---|---|---|
| 1. Influenza (Most Probable) | – Acute onset of fever, sore throat, fatigue, myalgia, dry cough, headache. – Sick contact with similar symptoms. – Missed flu vaccine. – Typical influenza-like illness presentation. | – No significant findings against, mild presentation, but classic symptoms. | Influenza typically presents with an abrupt onset of fever, muscle aches (myalgia), fatigue, sore throat, and dry cough. The combination of systemic (myalgia, fatigue) and respiratory (cough, sore throat) symptoms strongly supports this. |
| 2. Viral Pharyngitis (Non-influenza) | – Erythematous pharynx, sore throat, cervical lymphadenopathy. – Headache and mild fever are common in viral pharyngitis. | – Prominent systemic symptoms (fatigue, myalgia) suggest a broader viral illness. | Viral pharyngitis can cause sore throat and lymphadenopathy, but usually presents with milder systemic features compared to influenza. |
| 3. Streptococcal Pharyngitis (GAS) | – Sore throat, anterior cervical lymphadenopathy, pharyngeal erythema, fever. | – No tonsillar exudates, no rash, presence of cough (cough is uncommon in GAS). – Patient is older adolescent. | GAS pharyngitis is a key differential in sore throat cases, but the presence of cough and lack of tonsillar exudates make this less likely. |
| 4. COVID-19 Infection | – Respiratory symptoms (cough, sore throat), fatigue, headache. – Missed COVID booster. | – No anosmia, SOB, or loss of taste/smell. – Rapid symptom onset and sick contact pattern more typical of influenza. | COVID-19 can present similarly, but hallmark features (loss of smell/taste, dyspnea) are absent. Still possible but less likely. |
| 5. Infectious Mononucleosis (EBV) | – Sore throat, fatigue, anterior cervical lymphadenopathy. | – No posterior lymphadenopathy, splenomegaly, prolonged duration (>1 week). – Acute onset is less typical of EBV. | EBV commonly causes fatigue and sore throat but has a more insidious onset and posterior cervical nodes. Less likely here. |
Most Probable Diagnosis:
Influenza (Uncomplicated Influenza-like Illness)
Rationale:
- Classic triad: fever (38.3 °C), myalgias/fatigue, and dry cough present.
- Acute onset: Symptoms began suddenly 4 days ago after social exposure.
- Sick contact: Roommate with similar symptoms supports contagious viral infection.
- Unvaccinated: Missed annual flu vaccine increases susceptibility.
- Physical exam: Erythematous pharynx, cervical lymphadenopathy, tachycardia—typical findings in influenza infections.
- No red flags: No evidence of bacterial superinfection, severe respiratory compromise, or prolonged illness.
Guarantee 95%+ Scores on Your i-Human Case
Struggling with your i-Human case? Ivy Nursing Help ensures top-notch guidance for assured 95%+ scores. Excel effortlessly—order now and achieve outstanding results with expert nursing simulation support!
Clinical Impression on Marvin Webster iHuman
Marvin Webster’s presentation most strongly aligns with influenza—likely a mild to moderate case of uncomplicated influenza-like illness. Supportive care and patient education are appropriate, with no immediate need for further diagnostic testing or specialist referral.
Conclusion
- The Marvin Webster iHuman case highlights a classic presentation of an uncomplicated influenza-like illness in a young adult.
- Marvin Webster, an 18-year-old college student, presented with a 4-day history of sore throat, dry cough, fatigue, headache, and myalgia following social exposure and a sick contact.
- His history of missed influenza vaccination, fever, tachycardia, anterior cervical lymphadenopathy, and erythematous pharynx strongly supported a viral etiology, with influenza being the most probable diagnosis.
- This case highlights the importance of thorough history-taking, systematic symptom analysis using OLDCARTS, and focused physical examination to establish a working diagnosis efficiently.
- Patient education regarding hygiene, symptom management, and vaccination plays a crucial role in preventing complications and community spread.
- The Marvin Webster iHuman scenario serves as an excellent learning tool for nursing and healthcare students to practice clinical reasoning, differential diagnosis, and evidence-based management in common upper respiratory tract infections.
FAQs: NR509 Week 2 iHuman: Marvin Webster
What is the Marvin Webster iHuman Differential Diagnosis?
- Marvin Webster iHuman case involves evaluating common respiratory illnesses in health professions education.
- Differential diagnoses include:
- Influenza → Most probable; presents with fever, cough, sore throat, myalgia, and fatigue, often secondary to an infectious cause.
- Covid-19 (SARS-CoV-2) → Considered due to respiratory symptoms and missed booster, though classic loss of taste/smell is absent.
- Viral Upper Respiratory Infection → Common in student populations; includes viral or bacterial infections affecting the respiratory tract.
- Nursing document findings highlight key OLDCARTS data and physical exam clues for accurate assessment.
- Proper differential diagnosis in Marvin Webster iHuman supports evidence-based care, infection control, and accurate clinical reasoning.
- Emphasize follow-up in the student population to prevent complications and promote vaccination awareness.
What is the Marvin Webster iHuman Problem Statement?
- Patient Background
- Marvin Webster iHuman involves an 18-year-old male college student presenting for evaluation.
- Main symptoms: dry cough, sore throat, fatigue, headache, and myalgia lasting 4 days.
- Relevant Medical History
- Past medical history of childhood asthma (resolved).
- Missed annual influenza vaccine and COVID booster.
- Sick contact with a roommate showing similar symptoms.
- Physical Examination Findings
- Fever of 38.3 °C, tachycardia at 108 bpm.
- Bilateral anterior cervical lymphadenopathy.
- Erythematous pharynx without tonsillar exudates.
- Clinical Significance
- Presentation is consistent with viral respiratory infection, likely influenza, requiring focused assessment, education, and follow-up to prevent complications.
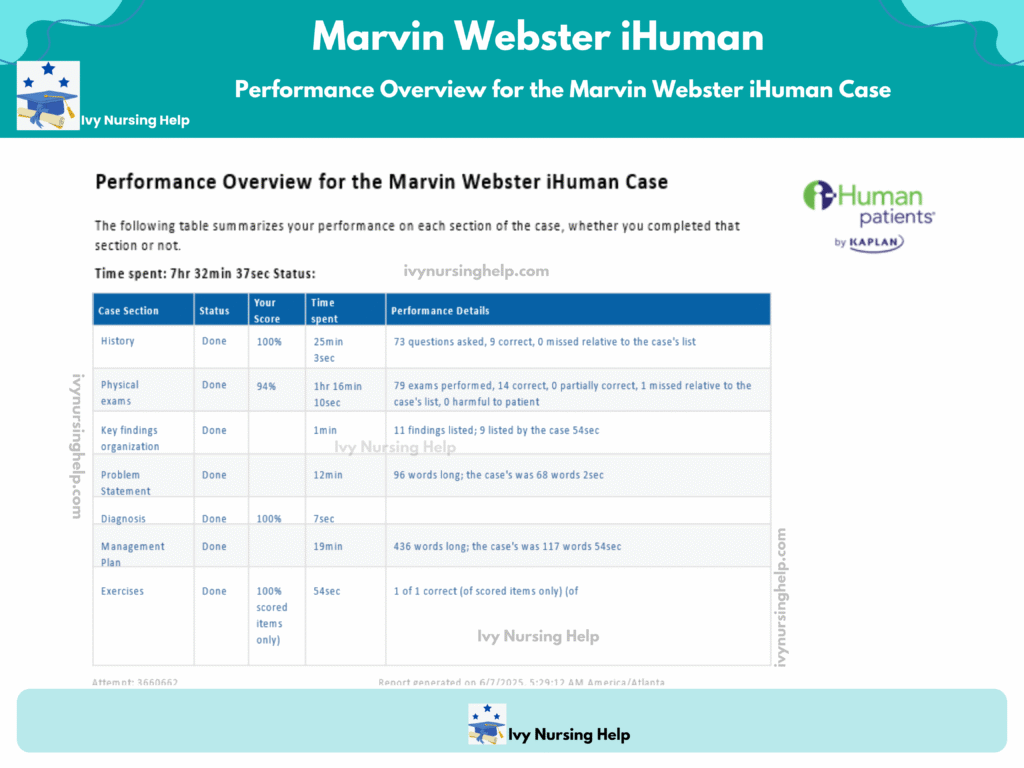
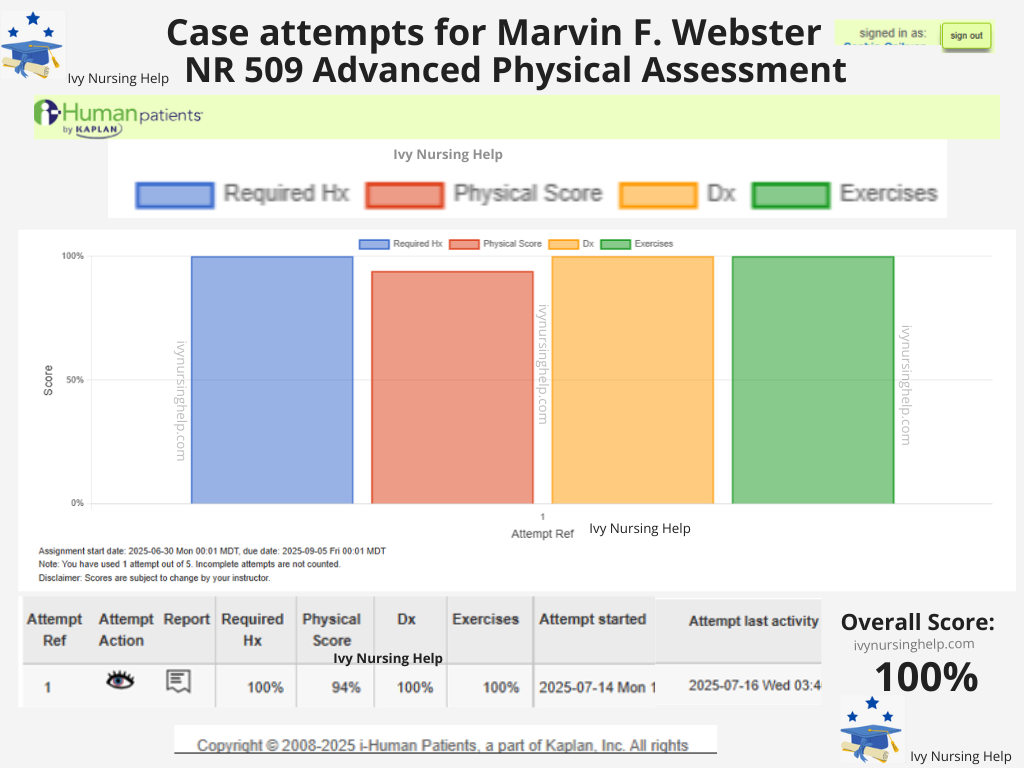
Assess your performance in creating and documenting a management plan in the Marvin Webster iHuman case.
- In managing the Marvin Webster iHuman case, I believe my performance in creating and documenting the management plan was thorough and well-structured.
- I effectively identified influenza-like illness as the most probable diagnosis and supported it with clear subjective and objective findings.
- I outlined appropriate medications, including acetaminophen and dextromethorphan/guaifenesin, and emphasized patient education on rest, hydration, hygiene, and vaccination follow-up.
- Additionally, I documented a clear follow-up plan to monitor progress and address potential complications.
- Overall, I applied clinical reasoning systematically, prioritized evidence-based care, and communicated the plan clearly, which are essential skills in nursing practice and patient management.
